Surgery vs chemoradiation
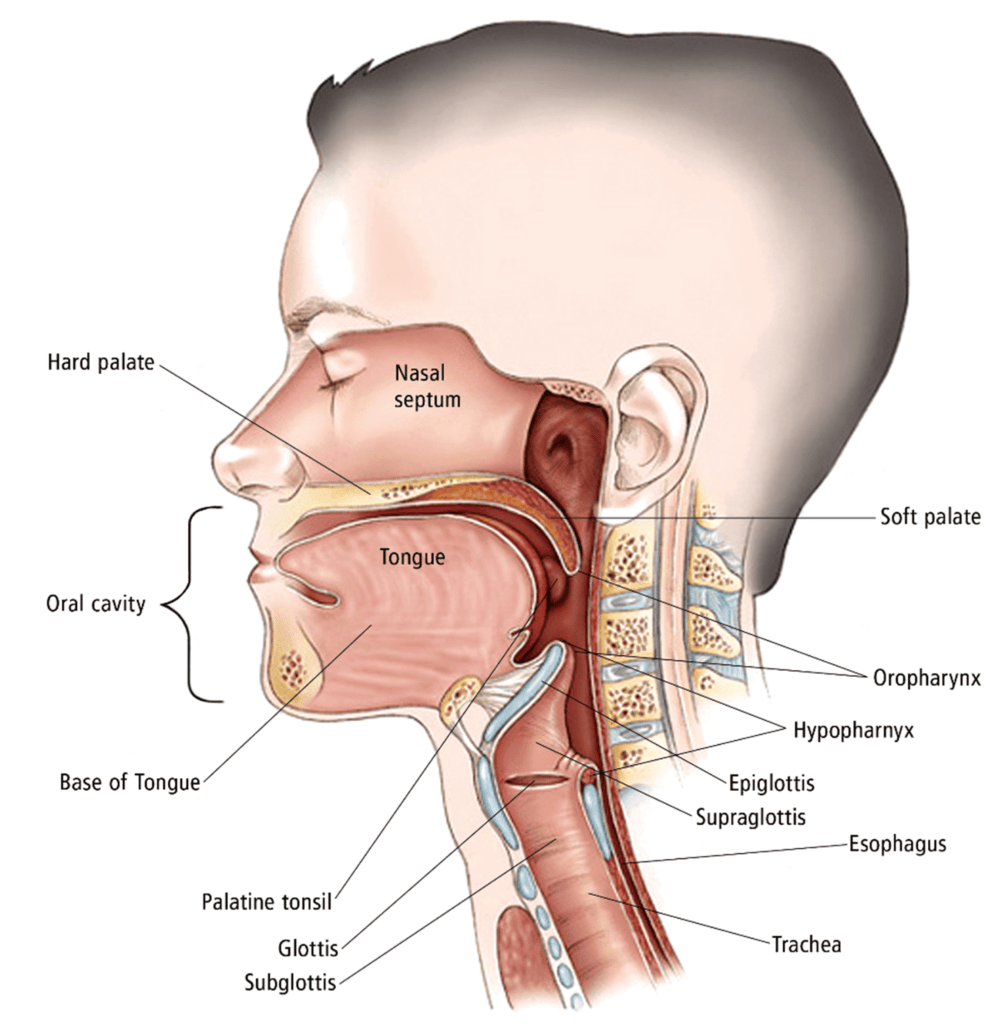
Old school surgery for head and neck cancers used to involve splitting the jaw bone in half just to approach tumors in the back of the throat. Ouch! Often, radiation and/or chemotherapy would be needed after surgery to sterilize the remaining microscopic disease as well. Upfront chemoradiation eventually was shown to effectively treat the cancer 80% of the time (with surgery reserved to salvage local recurrences), but 50% of patients still died from distant spread or other complications.
In 2004, robotic surgery was developed which allowed surgeons to resect tumors in the throat without splitting the jaw. Excellent outcomes were reported, but the number of specially trained surgeons is still limited today. ORATOR is the only randomized trial comparing definitive chemoradiation to robotic surgery. A surprising number of patients in the surgery arm needed additional radiation (71%) and/or chemotherapy (24%) after, negating the possible advantages of surgery alone. Robotic surgery is not currently offered for head and neck cancer patients in Reno. Patients are referred to UC Davis or Stanford for consultation if interested and are able to travel.
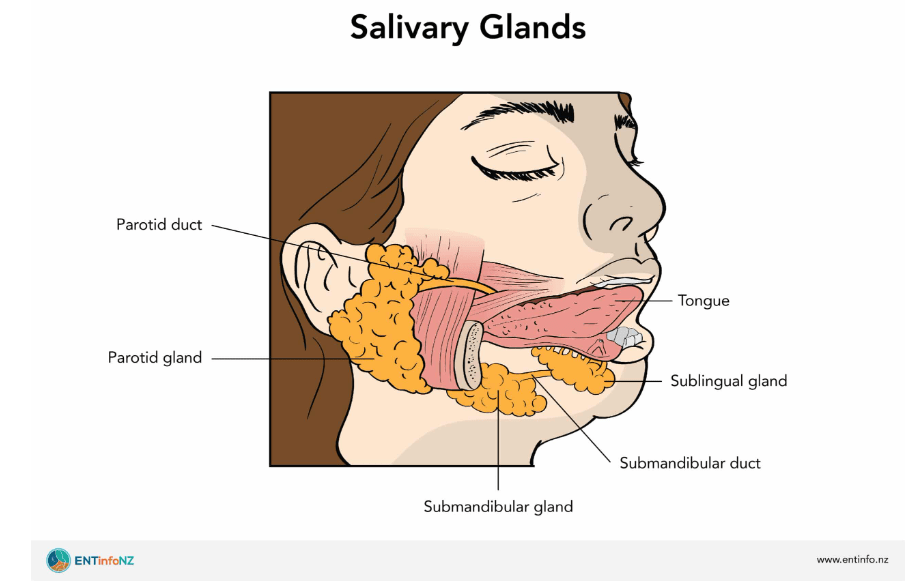
The most common long term side effects of head and neck radiation are dry mouth and difficulty swallowing, which significantly impact quality of life. In the past, smoking and alcohol related cancers proved to be hard to cure and a standard of 70Gy was prescribed to the gross disease and at least 50Gy was prescribed to the areas potentially harboring microscopic disease. Salivary glands stop functioning after 26Gy and swallowing muscles scar up around 45Gy.
New radiation technology allowed the first wave of de-escalation. IMRT made it possible to omit structures like the salivary glands from high dose radiation, reducing long term dry mouth. As doctors became more comfortable with the technology, low risk lymph node regions were avoided, pathologically node-negative necks were avoided, and this further reduced dose to the swallowing muscles and salivary glands.
Proton therapy
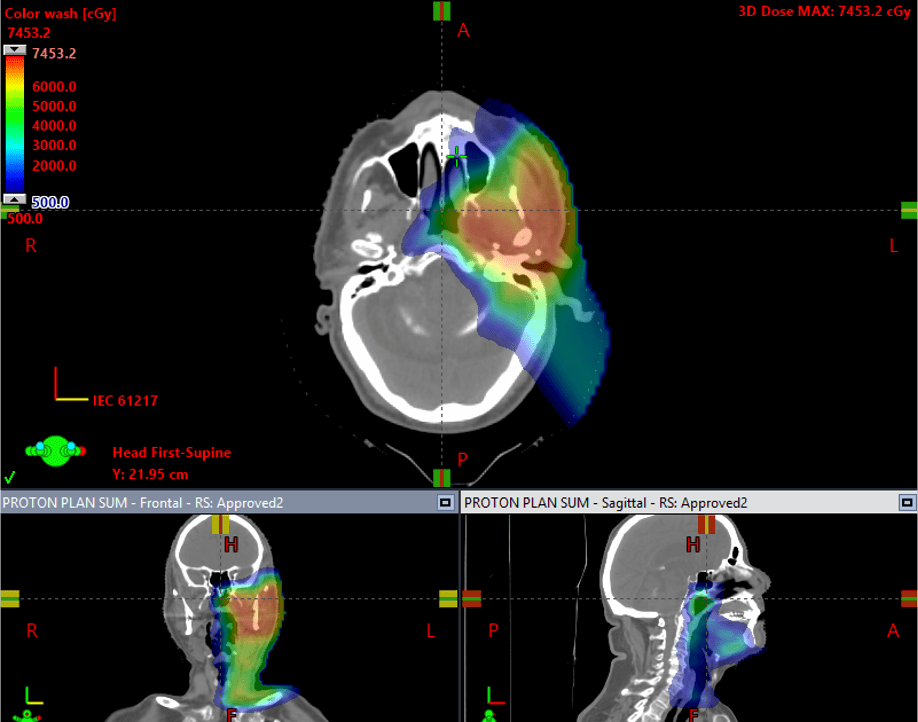
Proton therapy is especially useful if only treating one side of the neck. This is safely done in well-lateralized tonsil tumors or salivary gland tumors. The advantage of protons over X rays is the intermediate and low dose radiation to the uninvolved side can be negligible. A randomized trial comparing IMRT to proton therapy in head and neck cancers was recently presented at ASCO 2024, showing equivalent tumor control but less swallowing toxicity with protons. The closest proton centers to Reno are in southern California or Seattle due to the expense of building these cyclotrons.
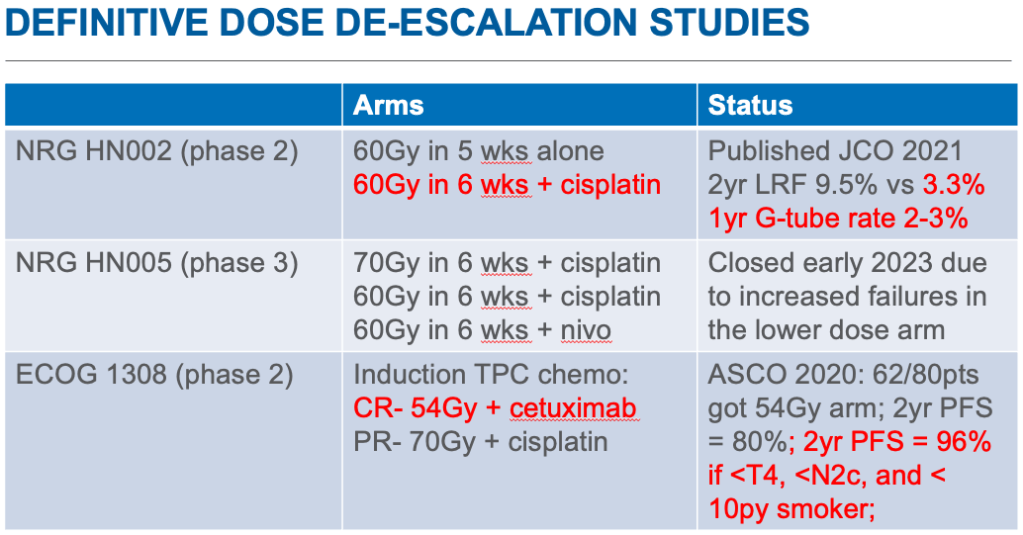
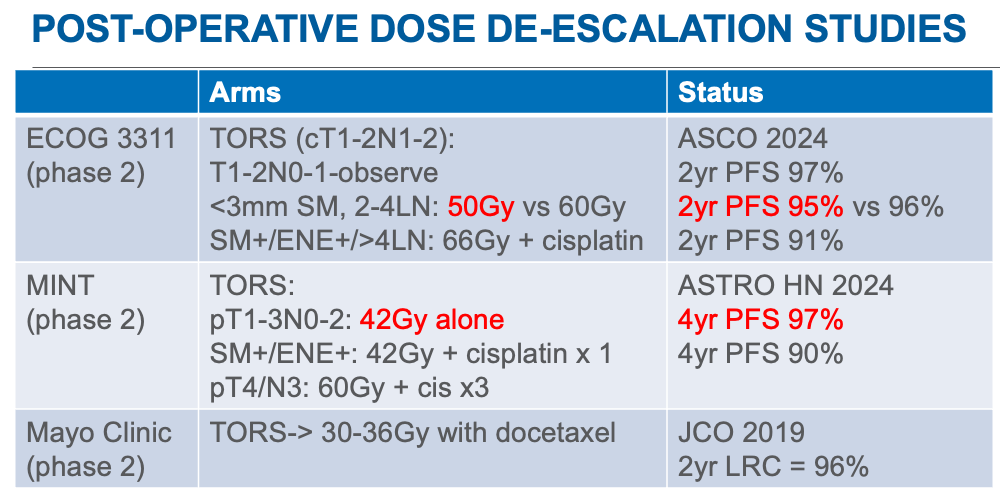
Dose de-escalation
Patient selection is the most important factor
The most prevalent type of throat cancer is now caused by the human papilloma virus (HPV). This virus is commonly spread by secretions such as saliva and normally cleared by our bodies. In some cases, the infection persists chronically undetected and eventually disrupts the infected cells’ growth regulation enough that cancer forms. During the process of diagnosis, a biopsy is taken and cells are stained for p16, a biomarker of HPV-caused cancer. HPV-caused cancers are highly curable and many trials have looked at reducing radiation doses to improve quality of life. However, results have been mixed. Large trials pragmatically only using p16 staining rather than HPV testing will include 5 (North America)-30% (Europe) HPV negative patients, who are less curable.
MSKCC Protocol
The group at Memorial Sloan Kettering Cancer Center has been the most aggressive and forward with their dose de-escalation for HPV-caused oropharyngeal cancers. Using FMISO-PET, they select patients without tumor hypoxia to de-escalate gross tumor radiation dose from 70Gy to 30Gy. Phase 2 results at ASCO 2024 have generated excitement for a phase 3 trial. In addition, since 2017 they have reduced the subclinical neck radiation dose to 30Gy as their standard of care. All patients get extensive imaging with FDG-PET, MRI, and CT neck with contrast to delineate gross involved disease. Two year results have shown only one elective nodal failure in 276 patients.
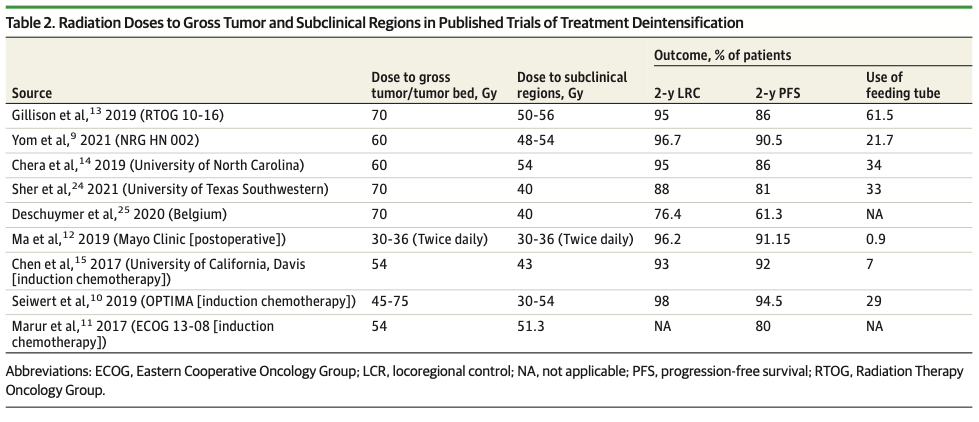
In summary, dose de-escalation is potentially a game-changer for well-selected patients. However, most patients we see in Reno are not able to travel for an FMISO PET or be considered for proton therapy. Even scheduling basic staging scans can delay starting therapy. The uncertainty in p16 staining/HPV status and smoking history also confounds our predictions. Thus to make a blanket lower dose prescription for gross disease could potentially lead to more local failures needing surgical salvage. To some patients, that may be a risk that they are willing to take.
I do think there is enough evidence from post-op and definitive radiation trials that 50Gy is adequate to sterilize microscopic disease in a p16+ oropharyngeal cancer patient. The 30Gy data is reassuring to allow aggressive sparing of the salivary glands and swallowing muscles when not abutting gross tumor. The future for patient selection may be in mid-treatment measurement of circulating tumor DNA or imaging. Current data is further summarized in this review.