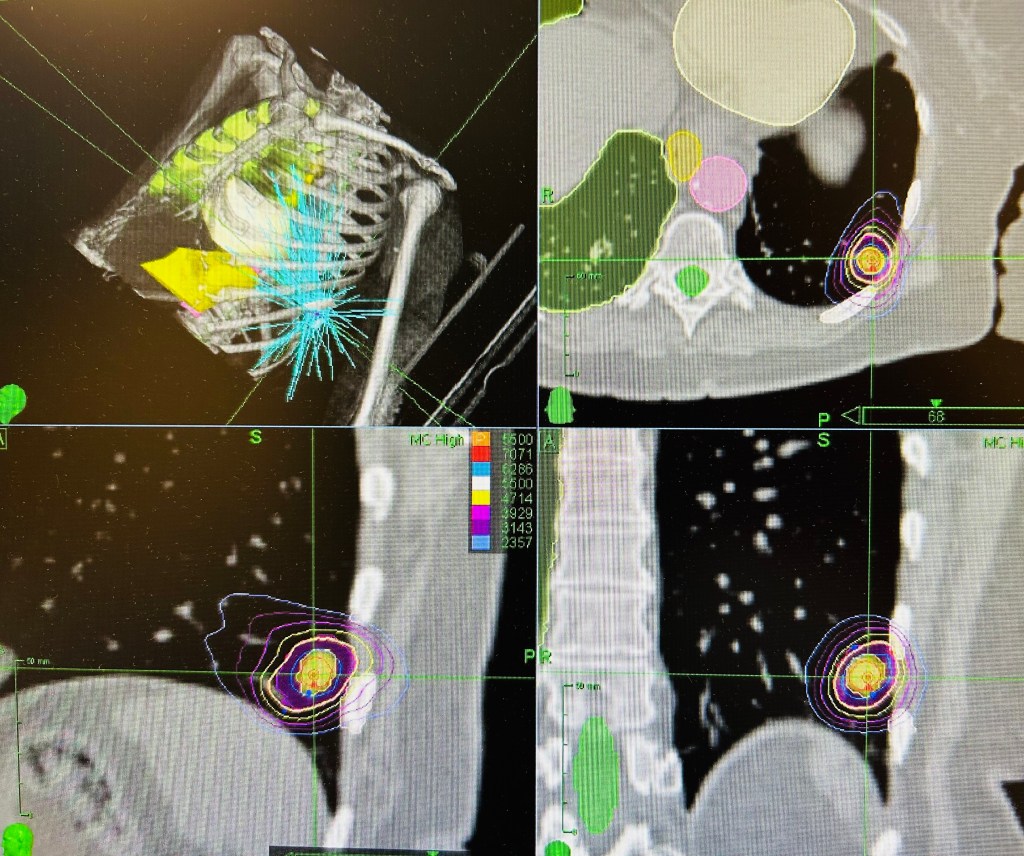
I read an excellent review of lung stereotactic body radiation therapy (SBRT) today from Drs. Buschberger and Videtic, outlining the history and future directions of non-invasive lung SBRT. Essentially, the 5 year local control is greater than 90%, but the rate of distant metastasis can be as high as 30%. In patients too frail for surgery, combining SBRT with immunotherapy shows promise and is being tested in at least three randomized trials.
For operable patients, an advantage of surgery is the opportunity for lymph node sampling to detect occult regional disease. However, pending the randomized trials (VALOR, STABLEMATES) between surgery and SBRT, my bet is survival differences will be negligible. This is because local disease recurrence rarely kills patients if surgical salvage is possible.
There was a good discussion of central vs peripheral tumors. While peripheral tumors can be safely treated in 1-3 high dose sessions, tumors within 2cm of the central lung structures should be treated in 5 sessions. The SUNSET trial recently gives us an 8 session treatment for “ultracentral” tumors touching the central lung structures. Importantly, respecting the normal tissue tolerance took priority over tumor dose.
Radiation pneumonitis is common after SBRT to the lung. Mostly seen on follow up CT scans 2-6 months after treatment, about 15% of patients present with a dry persistent cough of shortness of breath. A long course of steroids usually will resolve the symptoms. Patients with interstitial lung disease are at risk of SBRT worsening their lung function and need to balance the possible risks of dying from the cancer vs treatment (7.7% in ASPIRE-ILD).
As immunotherapy becomes prescribed more around SBRT, I’m sure we will start to see higher rates of radiation pneumonitis. Recent data from UPenn shows a doubling of symptomatic pneumonitis after consolidation immunotherapy became standard of care in the locally advanced lung cancer patients.