ADT alone vs ADT + RT
Before the 1990s, patients with high risk prostate cancer were thought to be incurable. Based on clinical and lab data, testosterone was found to be a driver of prostate cancer growth, and withdrawing testosterone could lead to cancer regression. Life-long castration with either surgery or hormone blockers like bicalutamide and eventually leuprolide, also known as androgen deprivation therapy (ADT), became a standard of care.
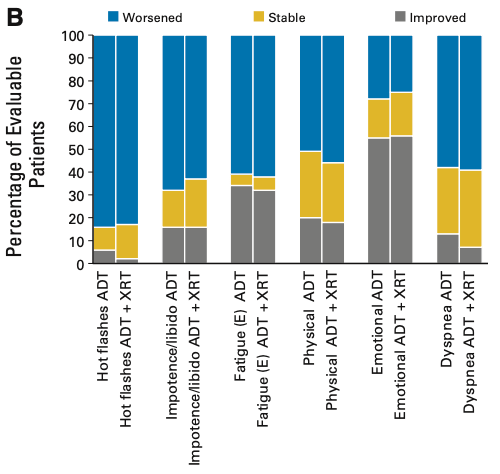
However, two randomized studies adding prostate radiation to ADT showed these patients were indeed curable, and radiation+ADT became the new standard. Quality of life on ADT is well documented on these studies, and multiple trials now give us a cost-benefit comparison for patients to consider. Compared to the transient side effects of radiation, ADT has a greater and more sustained effect in patient surveys.
Benefit of ADT with definitive RT
The MARCAP meta-analysis confirmed that ADT improved cure from PSA recurrence, reduced distant metastasis, and improved overall survival regardless of moderate radiation dose-escalation. The clinically meaningful endpoints of distant metastasis and survival were improved by an absolute risk of 9% and 8%, respectively. Most of the benefit was shown in high risk prostate cancer patients. In the supplement (shown below), a breakdown by NCCN risk group showed the number of men that need to be treated with ADT for one to benefit.
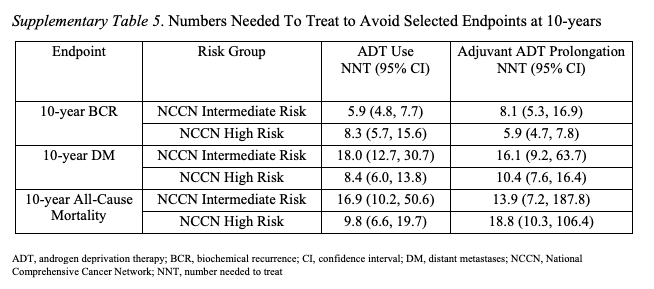
RTOG 0815 was not included in MARCAP but recent publication confirms the limited benefit of ADT in unselected intermediate risk patients treated with modern radiation. The 5 year risk of distant metastasis was 1% with ADT vs 4% without ADT. There was no difference in overall survival.
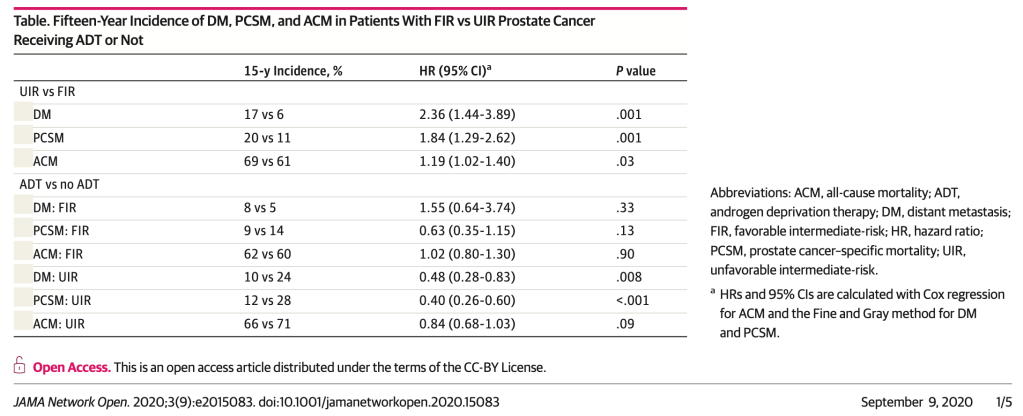
The NCCN guidelines define unfavorable intermediate risk as having a greater proportion of Gleason 4 disease compared to Gleason 3, or a large proportion of the prostate involved with cancer. A secondary analysis of RTOG 9408 using these criteria showed a larger benefit in these patient, and no benefit in the favorable intermediate risk patients. The table below shows the 15 year risks of distant metastasis, death from prostate cancer, and overall survival.
Benefit of ADT after prostatectomy
Previously, it was unclear whether radiation should be given right after prostatectomy in high risk patients or only with PSA recurrence. Three modern trials have shown about 60% of intermediate/high risk prostate cancer patients will be cured with surgery alone.
Of the remaining 40% that develop a rise in PSA after surgery, radiation with ADT can salvage 70-87% of them. Again, the benefit of ADT is highest in patients with high risk factors for distant metastasis. RADICALS-HD showed no meaningful benefit of 6 months of ADT with salvage radiation in a population of patients skewed to CAPRA-S intermediate risk 52%/high risk 33%. In a higher risk population (CAPRA-S intermediate risk 40%/high risk 52%), the 10 year metastasis free survival improved from 72% to 78% with 2 years of ADT. There was no difference in overall survival. The DADSPORT meta-analysis confirmed there is at most a 1-2% overall survival benefit and a predicted 8 year prostate cancer specific survival of 90% vs 94% with ADT. Most men would find these numbers underwhelming and choose to avoid ADT until PSA progression.
Better risk stratification?
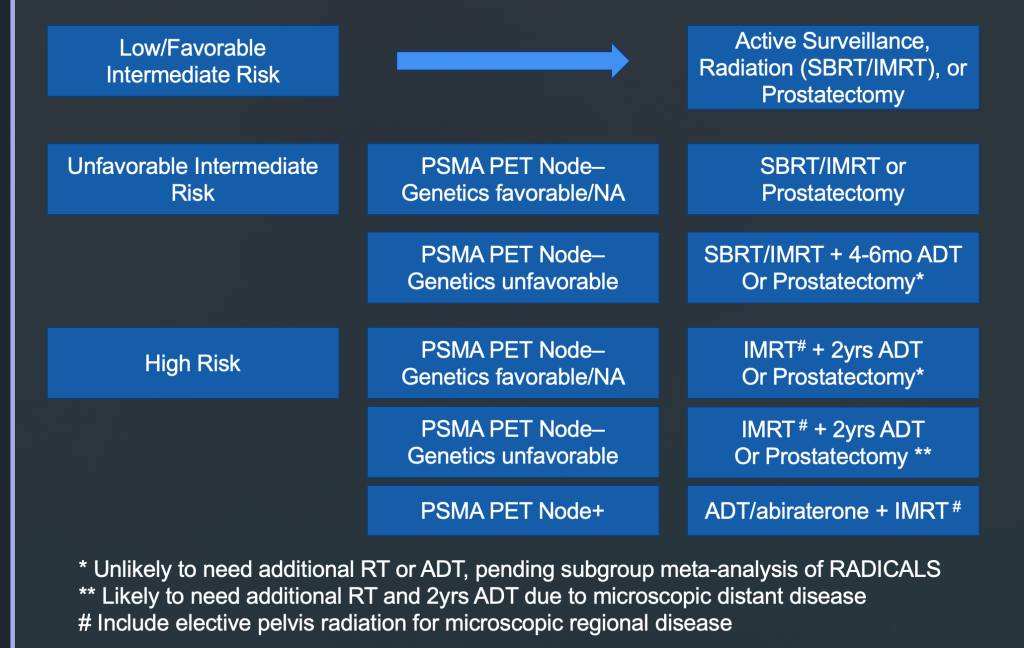
I think the logical conclusion is that ADT should be given for two years when there is a high risk for microscopic distant metastasis. There may be some benefit to 4-6mo of ADT in the unfavorable intermediate risk patients treated with definitive radiation, but not in patients treated with prostatectomy. Dose-escalation with brachytherapy likely is equivalent to prostatectomy in terms of local control, when patients are selected appropriately.
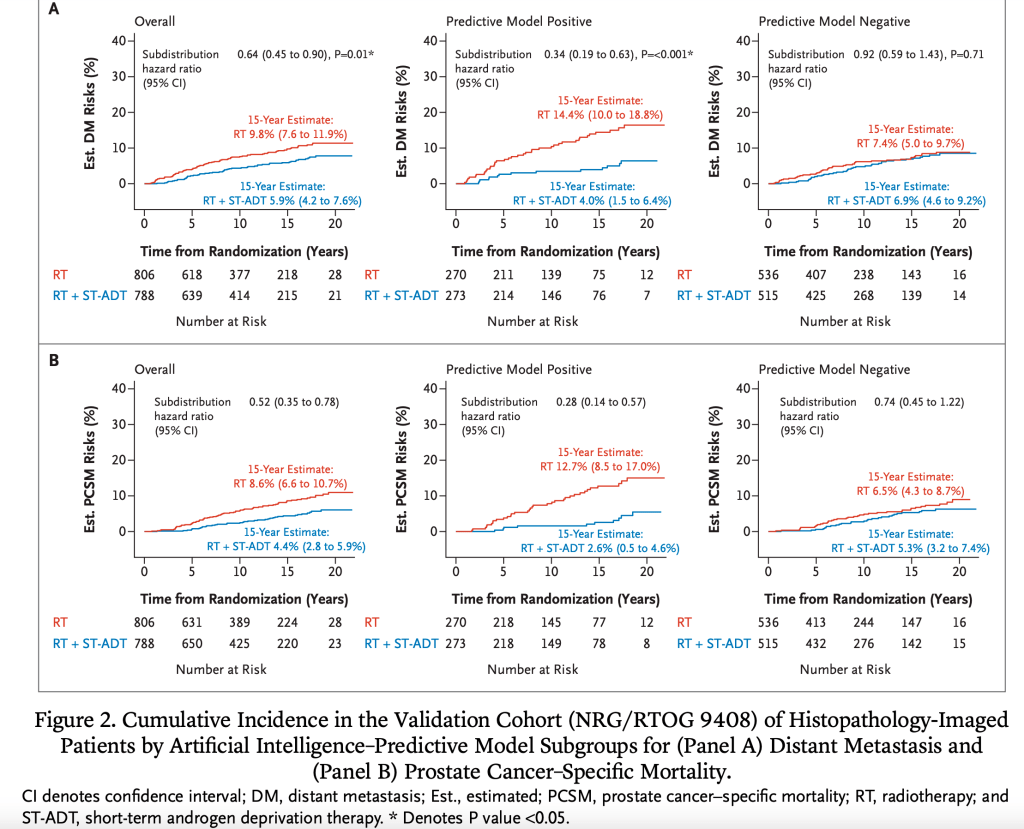
Tumor genetic sampling and artificial intelligence analysis offer additional risk information and should be obtained whenever possible. Secondary analysis of RTOG 9601 showed the 12 year overall survival benefit of 12 months ADT with salvage radiation was reduced in the low/intermediate Decipher risk group (2.4%) compared to the high risk group (8.9%). Early results of GU 006 validates a new genetic panel PAM50 to identify men who would benefit from ADT. Secondary analysis of RTOG 9804 with artificial intelligence also identified a subgroup of intermediate risk prostate cancer patients that benefit from 4 months of ADT with definitive radiation.
Testosterone recovery after ADT
Finally, patient preference and co-morbidities need to be taken into consideration. Testosterone levels may take years to return back to normal. MARCAP again gives some data in the table below on time to non-hypogonadal testosterone recovery (NHTR) and full testosterone recovery (FTR). A third of men will not have FTR.
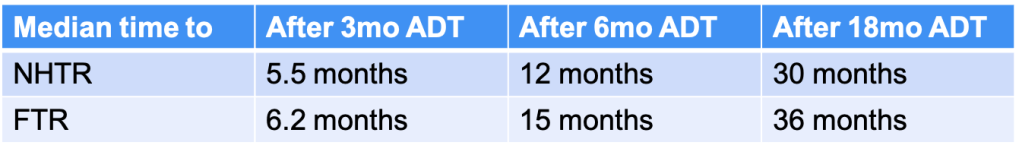
A new oral ADT called Relugolix allows patients to achieve normal testosterone levels on average 3 months after stopping ADT. For patients that have insurance drug coverage, Relugolix may be the golden bullet that gives maximum benefit without lingering side effects.