Low dose radiation therapy (LDRT) has had a resurgence in the radiation field recently, affectionately called the “healing rays”. Unlike radiation for cancer, the doses being used are much lower (0.3Gy to 10Gy LDRT compared to 60-70Gy for cancer) and expected side effects are minimal. Cell and animal studies have shown anti-inflammatory effects of LDRT, so it is like taking NSAIDs or steroids and non-invasively directing those effects to the problem area. I’m supportive of doctors studying the possible medical applications of LDRT, from COVID-19 to Alzheimer’s disease, but I wonder if there is an aspect of wishful thinking as well.
LDRT is increasingly being offered for osteoarthritis and musculoskeletal pain, even to world class athletes like Usain Bolt! Anecdotes are being shared of patients having life-changing improvements in pain. Indeed, LDRT has been offered for over 100 years and is commonplace in Germany. Multiple clinics publish a 60-90% improvement in pain scores that last 6-12 months, with about 40% of patients requiring a second treatment.
However, two prior sham-controlled (fake radiation vs real radiation) trials showed the results are exactly the same. Pain is notoriously difficult to study, and other accepted treatments such as steroid injections have also had negative trials.
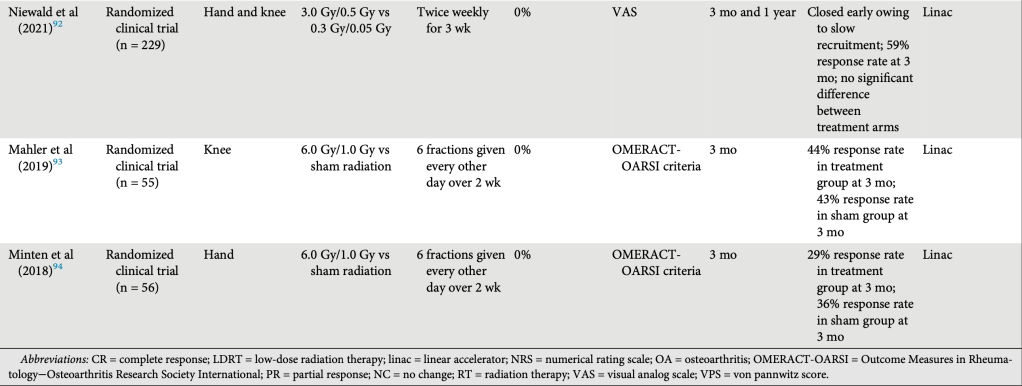
ArthroRad, the first listed study is actually a comparison of standard LDRT 3Gy with ultra low-dose RT 0.3Gy (equivalent to 300mSv or 50 CT scans). This was run by DEGRO, the German society for radiation oncology with the most experience using LDRT for osteoarthritis. Patients enrolled had symptoms on average 5 years, 70% had tried oral medications and 25% had tried injections. The mean pain score was 6/10 before treatment and 4/10 three months after treatment. The standard deviation was 2.5/10, meaning we can’t even statistically say there was ANY effect. About 60% of patients reported improved pain, 20% had stable pain, and 20% had worse pain. Subgroup analysis showed patients who had high baseline pain were more likely to report pain improvement. This is classic regression to the mean phenomenon.
Advocates will say that the cost of LDRT (~$2500) is much lower than say a knee replacement, and even if the relief is regression to the mean or placebo effect, patients are still happy. Perhaps there is a subgroup of patients that truly benefit and we just haven’t figured out who to include yet. There is a modern sham-controlled trial being done now, in Korea, and those early results were reported at ASTRO 2025.
Patients with painful knee osteoarthritis were split into three groups of 38 knees treated to either 3Gy vs 0.3Gy vs 0Gy ( sham placebo). They were only allowed to take Tylenol the first 4 months after radiation and surveys at 4 months showed a 78% vs 58% vs 42% response rate in the three groups, respectively. The trial will report 12 month results with more follow up.
Taken together, it seems 3Gy in 6 fractions is the therapeutic dose most likely to induce an effect. As high as 80% of patients will have some response compared to a 40% response rate with placebo. There have been no reported side effects or late secondary malignancies. LDRT may be an option for patients with mild to moderate osteoarthritis.