Dose escalation
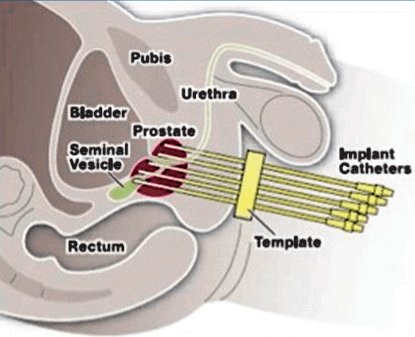
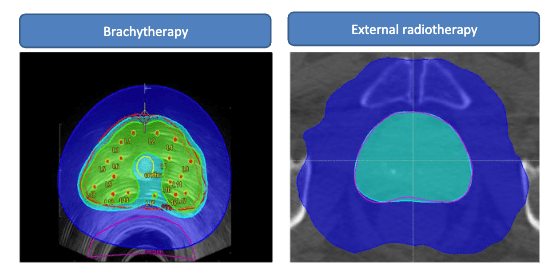
Brachytherapy involves positioning a radioactive source directly into the prostate. It is dependent on the skill of the doctor, but in experienced hands can give the most precise and accurate radiation delivery to the cancer. Since the sources are placed into the prostate, no extra margin of error is planned. Radiation dose falls off exponentially from the source, so the dose inside the tumor is extra high while dose to the rectum and bladder remain safe.
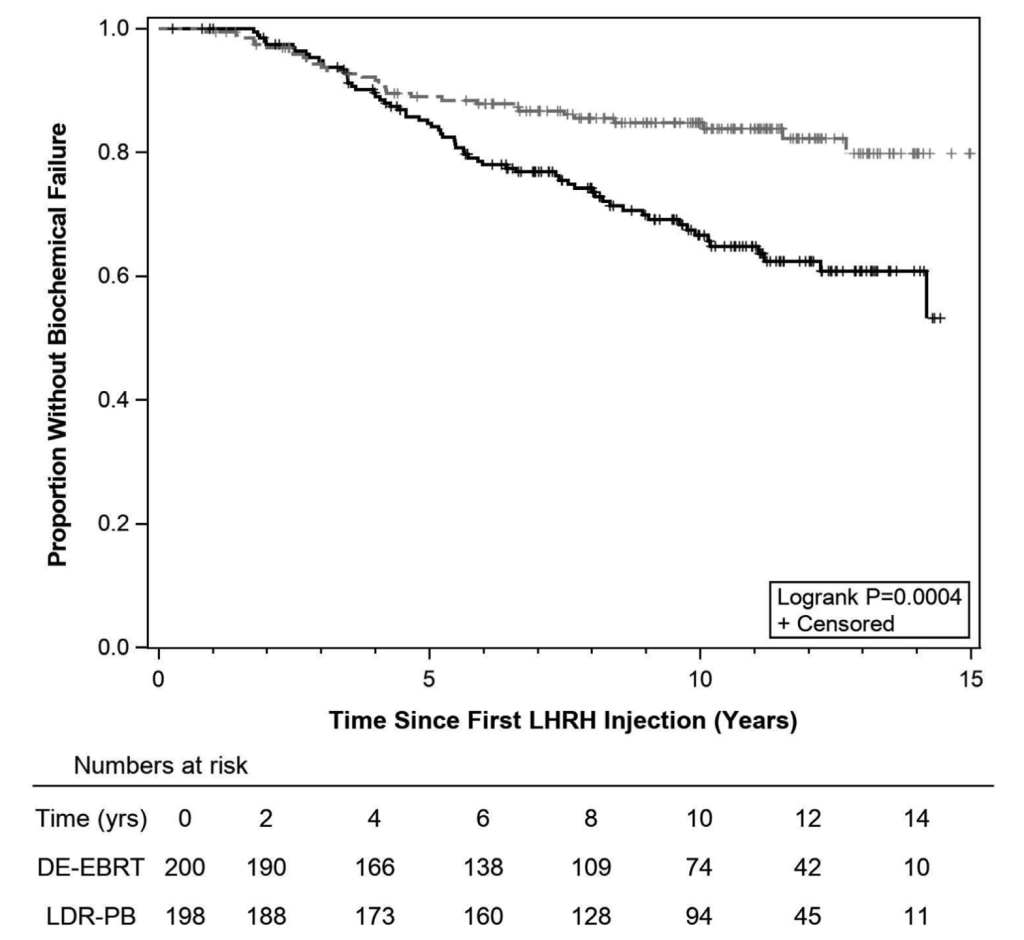
ASCENDE-RT compared giving extra boost dose radiation to the prostate with low dose rate brachytherapy versus external beam radiation. The brachytherapy kept PSA lower longer as shown below, but there was a trade-off in urinary side effects. Ultimately, there was no difference in distant spread of the prostate cancer or survival, perhaps as older men passed away from other diseases. This is an area of active study, but I think the patients that benefit most from dose-escalation with brachytherapy are younger patients that have high grade disease. The PSA becomes undetectable in a majority of prostate cancer patients treated with brachytherapy and SBRT compared to conventional fractionation alone, but it remains to be seen how this changes clinically meaningful outcomes.
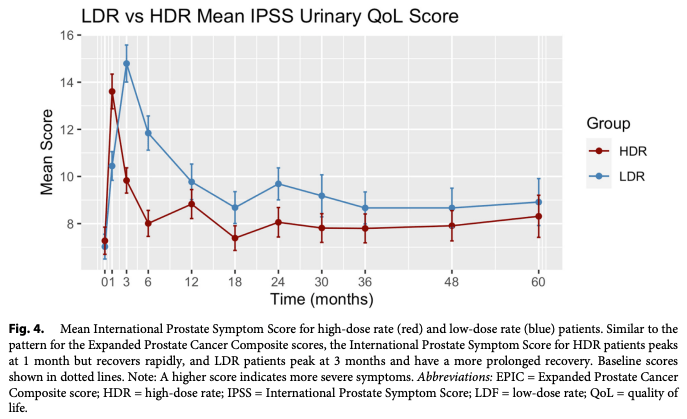
High dose rate (HDR) vs low dose rate (LDR) brachytherapy
LDR brachytherapy is sometimes called permanent seed implants because radioactive metal seeds are implanted and left in the prostate to give off radiation over months. HDR brachytherapy is a newer technique where catheters are implanted into the prostate temporarily, and a radioactive source is threaded through the catheters to deliver the radiation internally over minutes. After treatment, all the catheters are removed. HDR may allow a little more flexibility in delivering the radiation after the implant since the doctor can control which catheters and positions to dwell the radioactive source in. However, since the dose is delivered all at once, the urinary symptoms tend to be more intense for the first month. Afterwards, patient reported urinary and bowel quality of life are better with HDR vs LDR brachytherapy.