Conventionally fractionated IGRT-IMRT/VMAT
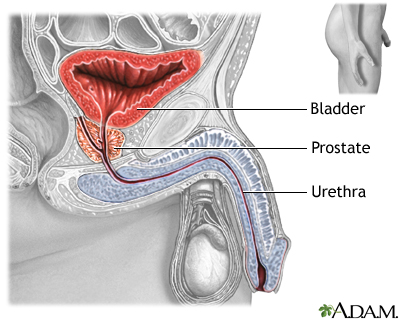
I mentioned in my previous post that modern radiation of the prostate now involves multiple beams from different angles so that the high-dose radiation hugs the prostate closer and falls off quicker around the rectum and bladder. Most modern machines will have a CT scanner attached so that the location of the prostate can be verified prior to each treatment. The prostate can move between treatments and even during treatment with breathing, coughing, passing gas, etc. Also, sometimes there is a big pocket of gas or stool in the rectum pushing against the prostate (and getting unnecessary radiation) that can be cleared prior to treatment if seen.

A typical margin for error with daily imaging can be accounted for by a 5-7mm expansion of the high dose region around the prostate. Prior to image-guidance, a 3D conformal plan may have had a 1-2cm margin and included large portions of the rectum and bladder. A total dose of 78Gy spread out over 39 treatments given once a day Monday through Fridays over 8 weeks is a reasonable approach that will kill the cancer and minimize side effects to the rectum and bladder. While daily treatments don’t last very long (typically 10 to 20 minutes commitment each day), some patients are still working or have an active lifestyle and would like to finish therapy quicker.
Moderately hypofractionated IGRT-IMRT/VMAT
In order to shorten treatment times, more dose needs to be given per day of radiation in order to cure the cancer (but the total dose needed decreases). A higher daily dose of radiation causes more damage to both the cancer and normal tissues, and the sub-lethal repair of normal tissues overnight may be incomplete. There was some concern by doctors that long-term scarring of normal tissues with the shorter treatments would lead to unacceptable side effects. Thus, the initial randomized studies compared conventional fractionation over 8-9 weeks with just slightly shorter hypofractionated courses over 4-6 weeks. There were several randomized trials showing equivalent cancer cure rates with the shorter treatments. The likelihood of diarrhea and urinary symptoms were about the same but occurred earlier during the hypofractionated radiation.
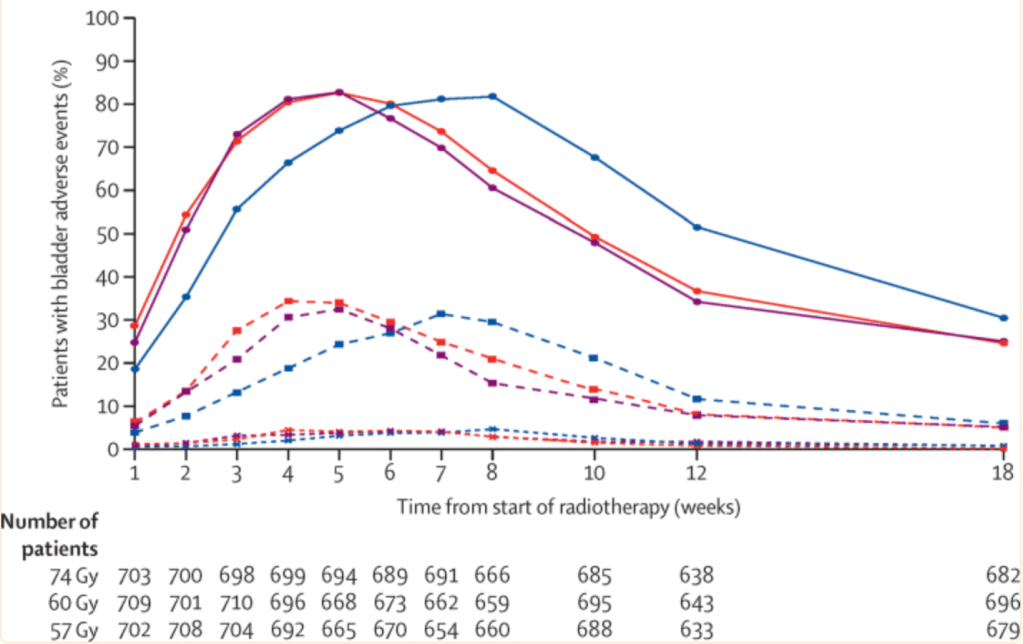
However, the rate of long term damage to the rectum and bladder/ urethra were slightly higher in some but not all of these trials. In RTOG 0415, the rate of prolonged rectal or bladder complaints increased 6-7% in the hypofractionated arm. The margins for error in these trials typically were 7-10mm as doctors were getting more comfortable with the daily imaging. Other trials looking at hypofractionation in high risk patients (and thus treating the entire seminal vesicles and more dose to the rectum) have also shown more late rectal bleeding, but not in all studies. Given the mixed results of trials, I suspect the larger margins and other technical aspects of the radiation plan made a difference. Moderately hypofractionated radiation is now commonplace in the US and may be offered for convenience.
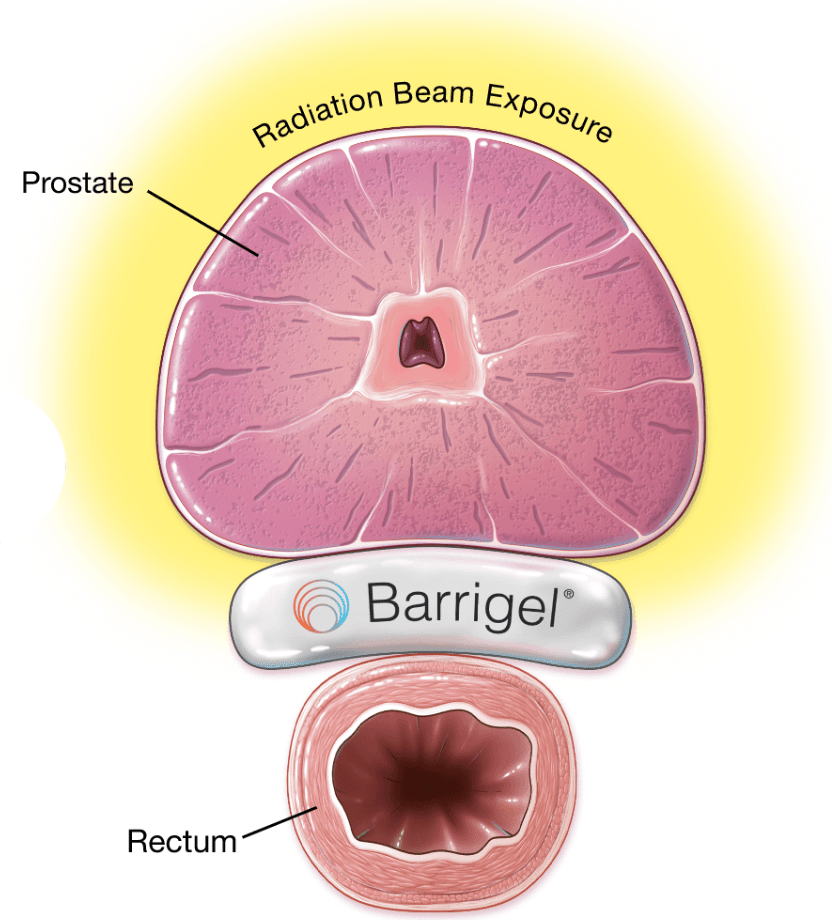
Hydrogel Spacers
A quick word about SpaceOAR and Barrigel. These are water-based gels that are injected in the space between the rectum and prostate. It can often be done the same time as metal fiducial markers are placed in the prostate for image tracking. There is minimal risk and the gel is reabsorbed in the body after 6 months. However, if the gel is placed in the wrong place and dissects the wall of the rectum, it can throw a wrench in your treatment. This has been reported a handful of times. Placing the hydrogels gives extra margin for error. It is like bowling with the bumper rails up.
Proton Therapy
The technologic advantage of proton therapy is there is no exit dose after the target is hit. These machines are expensive and limited to larger cities. The closest ones to Reno are in Seattle and San Diego. There has been a clinical trial accrued comparing IMRT photons vs protons (PARTIQoL) as well as a large registry of data being collected (COMPPARE), and early results show there are no differences in tumor control or quality of life. The question is whether exit dose matters when the prostate target is in the middle of the pelvis. The image below shows how some proton treatments are not very conformal to the prostate and still could treat just as much or more rectum/bladder. Not all proton centers are equal. The data from MD Anderson is very good if patients are able to travel and stay somewhere 6-8 weeks.

Stereotactic body radiation therapy with Cyberknife
This is where technology meets biology. Prostate cancer is relatively slow growing and responds best to high daily doses of radiation. What if there was a safe way to deliver this high dose radiation non-invasively, have the dose fall off rapidly outside the prostate, and account for prostate motion so we aren’t missing? Enter Cyberknife. The robotic arm allows radiation to be delivered in more directions/angles than a C-arm Linac. This allows for more precise radiation and rapid dose fall-off. In-room X rays track metal fiducials implanted in the prostate to adjust radiation delivery during treatment, allowing for submillimeter accuracy. The planned margin for error is 3-5mm.
Randomized studies comparing SBRT with conventionally or hypofractionated radiation such as HYPO-RT-PC and PACE B have shown no difference in 5 year prostate cancer cure rates (95% for low/intermediate risk, 84% for intermediate/high risk– neither trial allowed testosterone suppression). The urinary side effects are more pronounced and earlier with SBRT, but can be managed with medications such as Flomax or steroids in the 20-30% of men affected. The long term bladder or rectum side effects requiring medication occur at a rate of 5% or less.

Ultimately, we now know that 5 days of SBRT can cure cancer as effectively as 9 weeks of conventional radiation. Technology has enabled doctors to confidently reduce their planned margins for error, reducing unnecessary radiation to the rectum. I don’t routinely worry about rectal toxicity with Cyberknife. The inferior bladder and urethra still get a good dose of radiation, but these trials are showing that after the initial inflammation and swelling, recovery is better than we expected. Men now have such a range of choices when it comes to prostate cancer treatment. I haven’t even talked about brachytherapy and MRI-guided radiation. That will be next.