Early stage/low-intermediate risk cancer
The ProtecT trial randomized 1643 men with mostly low risk prostate cancer (but did include 24% intermediate risk and 10% high risk) to either active surveillance, prostatectomy, or conventional 3-D conformal radiation over eight weeks with six months of testosterone suppression.
Within two years, one out of every five men in the active surveillance group had radical treatment with either surgery or radiation. Within 10 years, nearly two out of every three men received radical treatment.
Interestingly, about 1/3 of patients that had surgery were found to have more advanced disease than initially thought, either with extension outside of the prostate or with higher grade cancer on final analysis.
After 15 years of follow up, only 3% of men died from prostate cancer, with no difference in which group they were assigned to. Surgery and radiation had the same cure rate in the prostate locally (90%) and in preventing spread to other parts of the body (5% risk). The risk of cancer spreading to other parts of the body increased slightly in men who waited to have radical treatment in the active surveillance arm.
Patient reported and functional quality of life differed based on treatment. Prostatectomy patients were more likely to have chronic urinary leakage and immediate erectile dysfunction from nerve damage compared to patients that receive radiation. Radiation increased the risk of prostate scarring around the urethra causing some obstruction, leading to waking up more times at night to urinate. Erectile dysfunction from radiation was more gradual, affecting about 70% of men after seven years and can be seen as acceleration of the normal process as men age. There was also increased rectal bleeding in the radiation group. Surgeons will say that surgical techniques have improved, and I can confidently say that radiation technology has improved since the time of the study, so the rate of side effects is likely less in both groups. However, this is the only large randomized study directly comparing surgery to radiation versus active monitoring and results have been quite revealing.
Intermediate/High risk prostate cancer
Here the discussion becomes even more interesting. There are no direct randomized comparisons of surgery versus radiation in patients with high grade disease, but surgeons argue that radiation can be given after surgery while they rarely operate after radiation. Surgery is essentially the same for low risk vs high risk prostate cancer, so the side effects are well-documented. Radiation for high risk disease is combined with two years of testosterone suppression, which increases side effects of hot flashes, fatigue, mood swings, and decreased libido. Radiation oncologists used to argue that all high risk patients would end up needing radiation and testosterone suppression after surgery (compounding side effects), but recent randomized trials may suggest otherwise.
The RADICALS-RT trial was recently published with 8 years of follow up. The trial randomized patients with mostly intermediate (55%) and high risk (37%) prostate cancer treated with prostatectomy and undetectable post-operative PSA to receive radiation to the prostate bed either within 6 months of surgery versus only if the PSA became detectable (>0.1). About a quarter of patients in each group also received testosterone suppression with radiation. As the figure below shows, 39% of patients eventually needed salvage radiation. I’d be curious to know if most of them were the high risk patients.
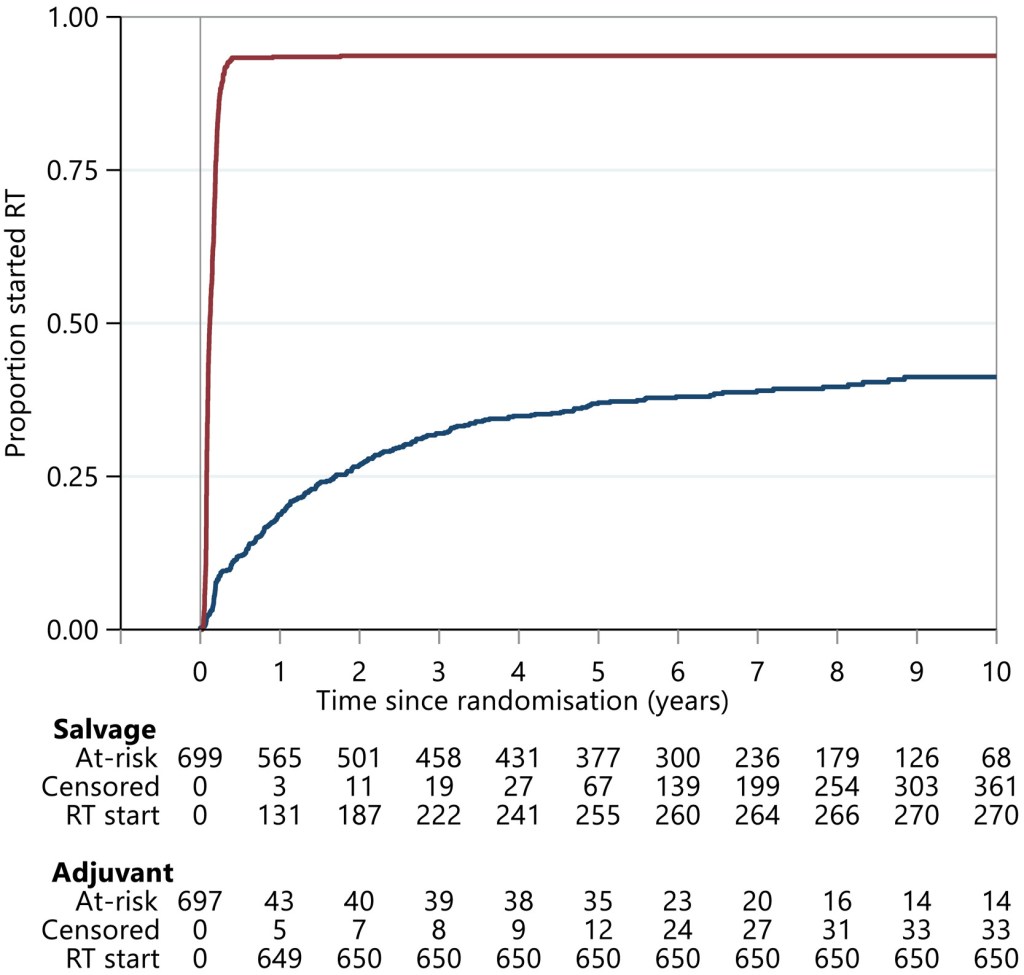
The results go on to show no difference in PSA failure after radiation (25% after 10 years), rates of distant spread (about 5% after 10 years), or death (8% after 10 years).
So what to make of this? Surgery alone cures about 60% of patients with intermediate-high risk prostate cancer. As long as PSA becomes undetectable after surgery, patients can wait (and often should to recover!) without any penalty. As other trials mature, we can eventually look specifically at the high risk patients separately from the intermediate risk patients. Maybe there is a subset of very high risk patients that benefit from triple therapy (surgery + radiation + testosterone suppression) compared to just radiation + testosterone suppression. Then again, maybe not. Patients selected for surgery tend to be younger and more fit so indirect comparisons on survival are unfair. It will take a randomized trial to decide.
In my next post, I’ll look at how modern radiation technology is enabling shorter and more convenient treatments. I think prostatectomy and modern radiation have excellent results with different side effect profiles for low and intermediate risk prostate cancer patients. The jury is still out in the high risk population, and patient preferences should always be considered. Thus, every prostate cancer patient should meet with both a surgeon and radiation oncologist to make the best treatment decision for him.